- All templates
- Use case diagrams
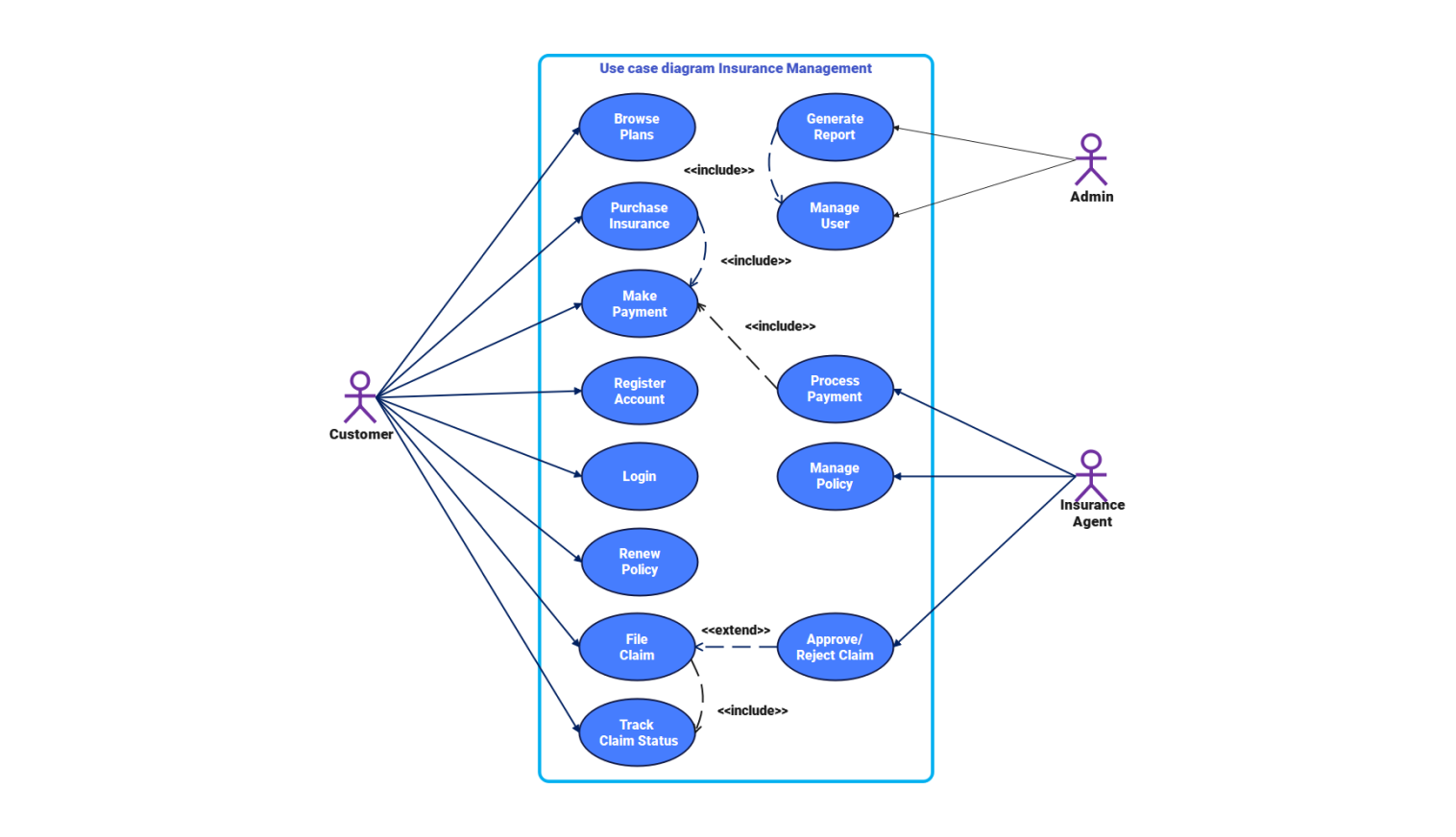
- Use case diagram insurance management
About this use case diagram for insurance management
The insurance management system runs through linked operations. These include policy creation, renewal, claim processing, and administrative tasks. First, a new user registers an account. This step stores customer details for later access. After registration, users log in to access services. They can browse available insurance plans. Each plan has key details like coverage type, duration, premium rate, and eligibility.
Users can review this info and then buy a chosen policy. Once a policy is selected, the purchase process begins with the payment. The payment function checks transaction details, processes online transfers, and confirms successful payments. After this, the policy is issued. After completion, the policy activates.
Users can then see their coverage and renewal dates. Renewal follows the same steps. Users can extend an existing policy by confirming the updated payment. The system manages claim activities. A customer can file a claim by providing details like policy number, claim type, and documents. The claim then enters review by an authorized insurance agent.
The agent checks the claim and eligibility. Then, they decide to approve or reject it. After that, the system updates the claim status. Users can track progress through their account dashboard. Administrative controls manage system upkeep and data consistency. The management module lets authorized staff update user accounts, check system activity, and create reports on policies, payments, and claims.
Each function works together. This ensures smooth data flow between registration, payment, claim handling, and reporting. This connects customers, agents, and admin tasks in the insurance management system. It creates a complete cycle.
Related templates
Get started with EdrawMax today
Create 210 types of diagrams online for free.
Draw a diagram free Draw a diagram free Draw a diagram free Draw a diagram free Draw a diagram free