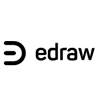
About this Pancreatic Beta Cell template
This diagram illustrates the complex process of insulin secretion within a beta cell. It visualizes how glucose enters the cell and triggers a series of chemical reactions to regulate blood sugar levels efficiently.
Glucose Entry and Metabolism
The process begins when glucose enters the cell through specific transporters. It then undergoes phosphorylation and metabolic cycles to create energy, which serves as a signal for the next steps in insulin release.
- GLUT2 Glucose Transporter
- Hexokinase IV Enzyme
- Glucose 6-phosphate
- Glycolysis Process
- Citric Acid Cycle
- Oxidative Phosphorylation
ATP Production and Channel Activity
Increased metabolism leads to higher ATP levels within the cell. This change affects specialized potassium channels, causing the cell membrane to depolarize. This electrical shift is crucial for activating the next phase of the secretion process.
- Intracellular ATP Accumulation
- ATP-gated K+ Channels
- Cell Membrane Depolarisation
- Hyperpolarisation Regulation
Calcium Influx and Secretion
The change in membrane voltage opens calcium channels, allowing ions to flow into the cell. This spike in calcium triggers the movement of insulin-filled granules to the cell surface, where they release insulin into the bloodstream.
- Voltage-dependent Ca2+ Channels
- Intracellular Calcium Increase
- Insulin Granule Transport
- Insulin Secretion via Exocytosis
FAQs about this Template
-
How do pancreatic beta cells detect high blood sugar?
Pancreatic beta cells detect high blood sugar through the GLUT2 transporter, which allows glucose to enter the cell proportionally to its concentration in the blood. Once inside, the glucose is metabolized into ATP. This increase in energy molecules acts as a primary signal, telling the cell that the body's blood sugar levels are elevated and need to be lowered immediately.
-
What is the role of calcium in insulin secretion?
Calcium acts as the final trigger for insulin release. When the cell membrane depolarizes due to closed potassium channels, voltage-gated calcium channels open. The resulting influx of calcium ions causes insulin-containing granules to fuse with the cell membrane. This process, known as exocytosis, releases insulin into the blood, allowing the body to process and store the circulating glucose effectively.
-
Why is the GLUT2 transporter important for these cells?
The GLUT2 transporter is vital because it has a high capacity for glucose, ensuring that the rate of glucose entry matches the blood's glucose levels. Unlike other transporters, GLUT2 allows the beta cell to act as a precise glucose sensor. This ensures that insulin is only secreted when sugar levels are high, preventing dangerous drops in blood sugar during fasting states.